Published online Jun 16, 2015. doi: 10.12998/wjcc.v3.i6.514
Peer-review started: January 16, 2015
First decision: February 7, 2015
Revised: February 24, 2015
Accepted: March 16, 2015
Article in press: March 18, 2015
Published online: June 16, 2015
Lymphangiomas are a group of benign malformations of the lymphatic system, and hemolymphangioma (or hemangiolymphangioma) is a rare congenital malformation of the lymphatic system with vascular involvement. These benign malformations are most commonly diagnosed at an early age, and may be present as a part of an associated syndrome. In this case report, we describe the first case of adolescent scoliosis associated with a large, paraspinous hemolymphangioma. A 15-year-old girl with an incidental finding of a paraspinous hemolymphangioma is presented along with her history, physical exam, radiographic findings, and operative course. The possible pathogenesis, treatment approach, and clinical dilemmas are also discussed. Given the well-known relationship between tumors and scoliosis, a benign paraspinous vascular and lymphatic tumor may be responsible for the presence of scoliosis in a small number of patients.
Core tip: This case report describes the first case of adolescent scoliosis associated with a large, paraspinous hemolymphangioma. Given the relationship between tumors and spinal deformity, a benign paraspinous vascular and lymphatic tumor may be responsible for scoliosis in a small number of patients.
- Citation: Swarup I, Bjerke-Kroll BT, Cunningham ME. Paraspinous hemolymphangioma associated with adolescent scoliosis. World J Clin Cases 2015; 3(6): 514-518
- URL: https://www.wjgnet.com/2307-8960/full/v3/i6/514.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i6.514
The association between paraspinous tumors and scoliosis is well recognized in clinical orthopaedics. To our knowledge, there are no reports in the current literature of an association between paraspinous hemolymphangioma and scoliosis. A lymphangioma is a congenital or post-traumatic malformation of the lymphatic system that is inherently benign, and typically found by palpation or with symptomatic compression of nearby anatomic structures. This entity has been classified into four types: capillary lymphangioma, cavernous lymphangioma, cystic lymphangioma (hygroma), and hemolymphangioma[1]. However, it may also be classified by cyst size as microcystic, macrocystic, or mixed[2].
Hemolymphangioma is the least common subtype, and has been found in the genitalia[3,4], gastrointestinal tract[5,6], head and neck[7,8], and extremities[9,10]. In the literature, there is also one report of a retroperitoneal hemolymphangioma without associated scoliosis[5], as well as a case series of bone lymphangioma associated with spinal deformity in the international literature[11]. Secondary transformation of lymphagioma to lymphangiosarcoma is rare, and when present, it is most often due to radiation therapy[12]. Treatment for symptomatic tumors includes marginal excision, aspiration and drainage, cryotherapy, injection of sclerosing agents, and radiotherapy[12]. However, recurrence is common, even after meticulous excision[10]. For asymptomatic lesions, a conservative approach may be taken in the form of serial imaging.
In this case report, we describe the first case to our knowledge of adolescent scoliosis associated with a large, paraspinous hemolymphangioma. The diagnosis and operative course of this patient is presented, in addition to a discussion of the pathogenesis and clinical management of this condition. We discuss various clinical dilemmas associated with this case, and we suggest a modification in the work-up of adolescent scoliosis in the setting of a strong family history of lymphatic tumors.
A 15-year-old girl presented for consultation regarding her scoliosis. Several years ago, the patient had been prescribed a brace for a 26-degree curve, but she admitted to non-compliance with this regimen. The patient was born at full-term by vaginal delivery. She had delayed puberty, and at the age of 15, she was 145 cm tall and weighed 34 kg. The patient was active in sports and did not complain of back pain. She had no family history of scoliosis or spine surgery. However, her maternal heritage was significant for several relatives with “hemangiomas,” including her mother who had a large and irregular lesion of the left upper extremity (Figure 1).
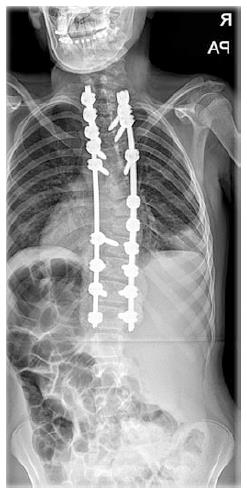
On physical exam, the patient demonstrated a right thoracic rib prominence of 10 degrees on Adams forward bending test. There were no cutaneous lesions present, and the remainder of her physical exam including neurological exam was unremarkable. Routine scoliosis radiographs were obtained (Figures 2 and 3), and demonstrated a right thoracic curve. No additional imaging was indicated at that time[13]. At this point, the patient’s presentation and curve pattern seemed consistent with adolescent idiopathic scoliosis (AIS), and given the severity of disease, the patient was indicated for a posterior spinal fusion from T2 to L1.
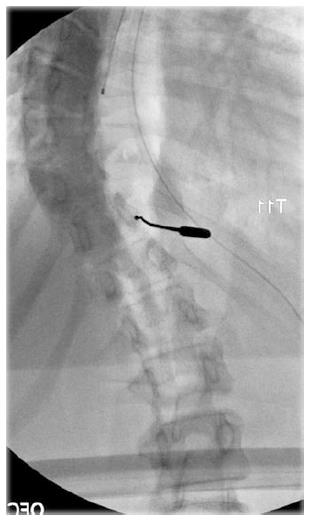
In the operating room, a standard posterior approach to the spine was performed, and the posterior elements were exposed. A Lenke probe was used to instrument the right pedicle of T11 (Figure 4), at which point, an immediate flow of thin, white fluid was noted through the tract. As a result, cultures were obtained, a drain was placed, and a decision was made to postpone the definitive procedure until the etiology of this fluid was determined.
The intra-operative Gram stain and microscopic analysis demonstrated moderate white blood cells without the presence of bacteria. Similarly, AFB, fungus, aerobic and anaerobic cultures were negative for any organisms. An magnetic resonance imaging (MRI) was also obtained that demonstrated a multilobulated, prominently vascularized lesion in the retroperitoneum from T7 to L5 (Figures 5 and 6). These pathologic and radiographic findings were reviewed with an expert pediatric surgical oncologist at a leading cancer center, and based on the patient’s strong family history, intraoperative finding of lymph, and the lesion’s characteristics on advanced imaging, a diagnosis of hemolymphangioma was made by the specialist. At that point, there was no indication for acute oncologic management, and there were no contraindications to proceeding with spine surgery. After discussion with the patient and her family, the decision was made to move forward with the definitive procedure. The patient underwent an uncomplicated posterior spinal fusion from T2 to L1 as previously planned (Figure 7). Care was taken to avoid the left pedicles of T7 to T9, as these levels corresponded to the largest portion of the hemolymphangioma seen on MRI. The patient recovered uneventfully, and was discharged without further incident. She was advised to follow-up with a pediatric oncologist for further surveillance and management. At one-year follow-up, the patient reported no symptoms, and her most recent radiographs revealed a stable correction with intact hardware.
At the patient’s initial presentation, the curve pattern and clinical behavior of her spinal deformity seemed consistent with AIS. However, the immediate proximity of this large malformation to the spine suggests an association with the patient’s spinal deformity, and warrants further discussion regarding the etiology and management of this patient’s scoliosis.
Several tumors within the spine have been shown to be associated with scoliosis and spinal deformity, most commonly osteoid osteoma and osteoblastoma[14,15], but also astrocytoma, ependymoma, epidermoid cyst[16], and bone lymphangioma[11]. However, there have been no reports of spinal deformity associated with paraspinous hemolymphangioma. In the case of osteoid osteoma and osteoblastoma, the tumor is more commonly located on the concavity of the curve. As a result, the deformity is caused by an asymmetric inflammation of the paraspinal muscles leading to asymmetric spasm[17]. In the case of bone lymphangioma, the spinal deformity is thought to result from a loss of spinal stability[11]. This patient’s tumor was also predominantly located on the concavity of the curve and her spinal stability was compromised suggesting a similar pathogenesis. In addition to an asymmetric inflammatory response and loss of spinal stability, unilateral disruption of growth or alteration of soft tissue dynamics may also have played a role in the pathogenesis of this patient’s spinal deformity.
This case also presents several interesting clinical dilemmas. The first dilemma is whether an MRI should have been obtained pre-operatively. Since this patient was healthy and lacked any neurological signs or atypical features, a pre-operative MRI did not appear to be indicated[13]. However, given the findings of this case report, it is reasonable to obtain a pre-operative MRI in patients with a strong family history of lymphatic tumors. Secondly, the unexpected intra-operative finding of a thin, whitish fluid from the pedicle raises an important dilemma regarding surgical decision-making. In this instance, a drain was placed and the etiology was further investigated. The staged procedure allowed the surgeon to review the patient’s case with experts and colleagues, and proceed when malignancy and infection were ruled out. Once the clinical diagnosis of a benign lesion was made, the surgeon was able to safely proceed with the planned procedure. Ultimately, this patient’s treatment was similar to the originally prescribed surgical management, with the exception of fewer pedicle screws being included in her instrumentation. Lastly, it is unclear whether the patient will benefit from treatment of her hemolymphangioma, since the natural history of this condition is benign and there are several risks associated with treatment, including malignant transformation and a high likelihood of recurrence[10,12]. Nevertheless, it is clear that this patient will require close follow-up to monitor for symptoms as well as recurrence of her deformity.
Overall, this case report describes the first case of a paraspinous hemolymphangioma associated with adolescent scoliosis. The natural history of hemolymphangioma is typically benign, however, it may be associated with the development of scoliosis in a small number of patients. The diagnostic work-up and surgical management of scoliosis may need to be modified in patients with a known history or strong family history of lymphatic tumors.
We would like to thank Michael P La Quaglia, MD, for his expertise in the oncologic diagnosis and management of this patient.
A 15-year-old girl presented with scoliosis.
On physical exam, the patient had a right thoracic rib prominence of 10 degrees on Adams forward bending test, she had no cutaneous lesions, and her neurological exam was unremarkable.
The possible diagnoses included adolescent idiopathic scoliosis or pathologic scoliosis.
The patient’s initial radiographs demonstrated a right thoracic curve, and magnetic resonance imaging (MRI) demonstrated a multilobulated, prominently vascularized lesion in the retroperitoneum from T7 to L5.
The intra-operative Gram stain and microscopic analysis demonstrated moderate white blood cells without the presence of bacteria, and AFB, fungus, aerobic and anaerobic cultures were negative for any organisms.
After consultation with an expert pediatric oncologist, the patient underwent a posterior spinal fusion from T2 to L1. However, care was taken to avoid the left pedicles of T7 to T9 as these levels corresponded to the largest portion of the hemolymphangioma seen on MRI.
There have been no previous reports of adolescent scoliosis associated with a large, paraspinous hemolymphangioma, however there have been several reports of spinal deformity associated with spinal tumors.
Hemolymphangioma is a rare congenital malformation of the lymphatic system with vascular involvement.
This case report presents the diagnostic work-up and surgical management of adolescent scoliosis associated with a large, paraspinous hemolymphangioma. Several clinical dilemmas are also discussed such as the need for advanced imaging, surgical decision-making, and post-operative management. An MRI may be indicated in patients with a strong family history of lymphatic tumors, and close collaboration with a surgical oncologist and other colleagues is required to ensure an optimal surgical outcome.
The case is rare, and the correction is well done. It is a nice paper.
P- Reviewer: Plaszewski M, Wang Y S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Landing BH, Farber S. Tumors of the cardiovascular system. Atlas of tumor pathology, Armed forces Inst Path. Washington, DC. 1956;. [Cited in This Article: ] |
| 2. | Giguère CM, Bauman NM, Smith RJ. New treatment options for lymphangioma in infants and children. Ann Otol Rhinol Laryngol. 2002;111:1066-1075. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 89] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Sapountzis S, Singhal D, Chen HC. Radical resection and reconstruction with bilateral gluteal fold perforator flaps for vulvar hemangiolymphangioma. Int J Gynaecol Obstet. 2013;121:179-180. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Shin YS, Doo AR, Kim MK, Jeong YB, Kim HJ. Cavernous Hemangiolymphangioma of the Testis without Cutaneous Hemangiomatosis in an Elderly Patient. Korean J Urol. 2012;53:810-812. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Kanaitsuka T, Itani K, Shigeta H, Yamamura Y, Kogawa T, Yoshikawa T, Sugino S, Kanatsuna T, Kondou M, Takashina K. [A case report of giant retroperitoneal hemolymphangioma]. Nihon Naika Gakkai Zasshi. 1987;76:1595-1603. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Vecchio R, Bakhtri M, Shebani A, Minona E, Gelardi V, Barbaros U. Incidental paracaval retroduodenal hemangiolymphangioma in adult patient: report of case removed laparoscopically. Surg Laparosc Endosc Percutan Tech. 2009;19:e8-e10. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Vilalta J, Mascaro JM. Hemangiolymphangioma of the tongue treated by transfixion technique. J Dermatol Surg Oncol. 1985;11:168-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Grasso DL, Pelizzo G, Zocconi E, Schleef J. Lymphangiomas of the head and neck in children. Acta Otorhinolaryngol Ital. 2008;28:17-20. [PubMed] [Cited in This Article: ] |
| 9. | Cole DJ, Sood SC, Broomhead IW. Pulmonary embolism associated with hemolymphangioma of lower extremity. Plast Reconstr Surg. 1979;63:265-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Kosmidis I, Vlachou M, Koutroufinis A, Filiopoulos K. Hemolymphangioma of the lower extremities in children: two case reports. J Orthop Surg Res. 2010;5:56. [PubMed] [Cited in This Article: ] |
| 11. | Wang YN, Zhang XJ, Qi XY, Sun L, Li CX, Sun BS, Bai YS, Yu FZ. [Diagnosis and treatment of bone lymphangioma associated with spinal deformity in children]. Zhonghua Yixue Zazhi. 2010;90:2701-2703. [PubMed] [Cited in This Article: ] |
| 12. | Chung KC, Kim HJ, Jeffers LL. Lymphangiosarcoma (Stewart-Treves syndrome) in postmastectomy patients. J Hand Surg Am. 2000;25:1163-1168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Do T, Fras C, Burke S, Widmann RF, Rawlins B, Boachie-Adjei O. Clinical value of routine preoperative magnetic resonance imaging in adolescent idiopathic scoliosis. A prospective study of three hundred and twenty-seven patients. J Bone Joint Surg Am. 2001;83-A:577-579. [PubMed] [Cited in This Article: ] |
| 14. | Burn SC, Ansorge O, Zeller R, Drake JM. Management of osteoblastoma and osteoid osteoma of the spine in childhood. J Neurosurg Pediatr. 2009;4:434-438. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Saifuddin A, White J, Sherazi Z, Shaikh MI, Natali C, Ransford AO. Osteoid osteoma and osteoblastoma of the spine. Factors associated with the presence of scoliosis. Spine (Phila Pa 1976). 1998;23:47-53. [PubMed] [Cited in This Article: ] |
| 16. | Bouaziz M, Daghfous M, Ladeb M. Childhood scoliosis revealing spinal cord tumors. Eur J Orthop Surg Traumatol. 2006;16:318-321. [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Akbarnia BA, Rooholamini SA. Scoliosis caused by benign osteoblastoma of the thoracic or lumbar spine. J Bone Joint Surg Am. 1981;63:1146-1155. [PubMed] [Cited in This Article: ] |